Free Living Will Form for Utah
Navigating the complexities of end-of-life decisions can be stressful for both individuals and their families. The Utah Living Will form serves as a crucial legal document designed to communicate one’s wishes regarding medical treatment in scenarios where they are unable to express themselves due to severe illness or incapacity. This form, part of a broader category known as advance directives, allows individuals to delineate their preferences about the use of life-sustaining treatments, including artificial nutrition and hydration, in certain medical conditions. Unique to Utah, this document not only helps to ensure that a person’s medical treatment preferences are honored but also relieves family members from the burden of making these difficult decisions in times of emotional stress. By completing a Living Will, individuals gain the opportunity to make thoughtful, personal decisions about their health care future, thereby providing clarity and peace of mind to themselves and their loved ones.
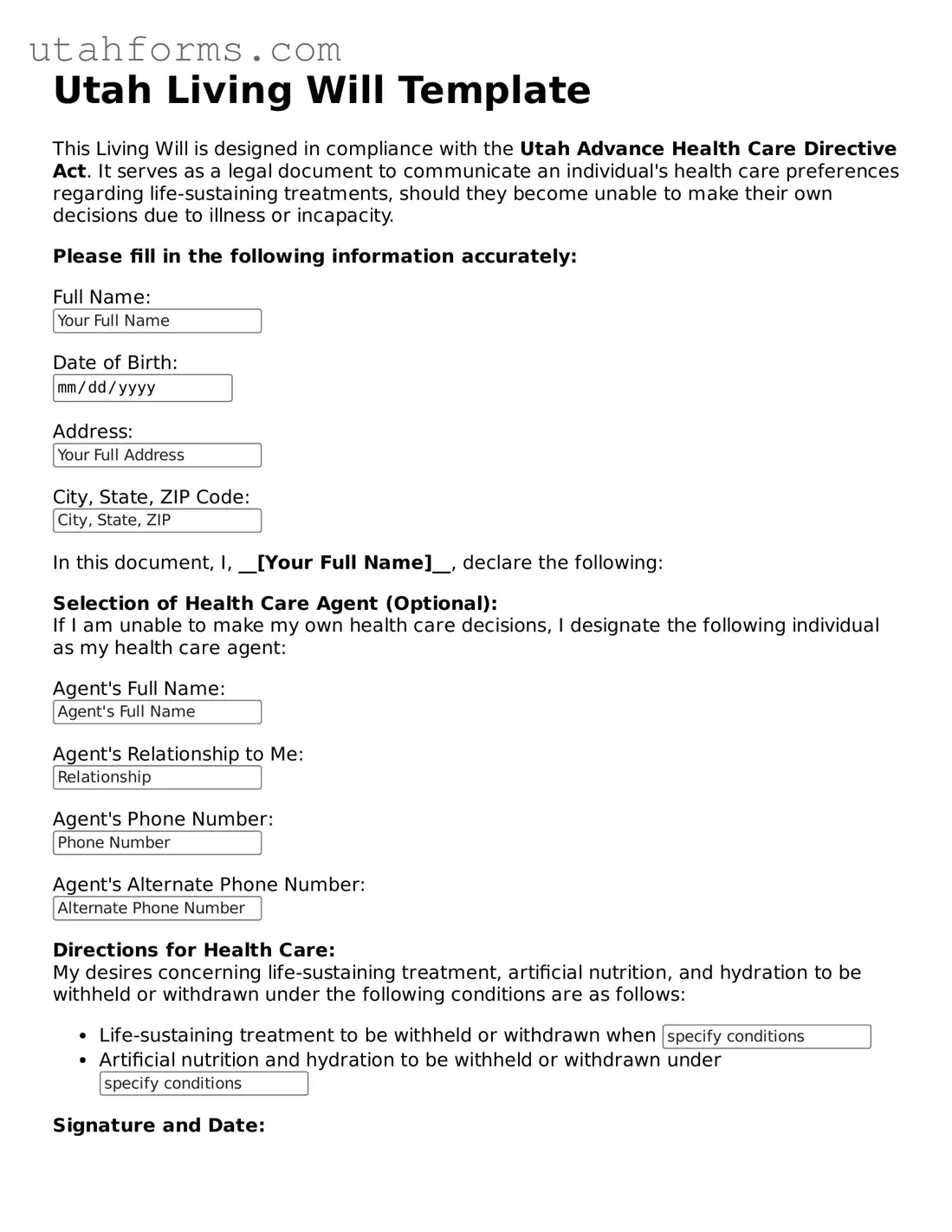
Preview - Utah Living Will Form
Utah Living Will Template
This Living Will is designed in compliance with the Utah Advance Health Care Directive Act. It serves as a legal document to communicate an individual's health care preferences regarding life-sustaining treatments, should they become unable to make their own decisions due to illness or incapacity.
Please fill in the following information accurately:
Document Properties
| Fact | Detail |
|---|---|
| Definition | A Utah Living Will is a legal document that outlines an individual's decisions about their medical treatment preferences in situations where they are unable to communicate due to illness or incapacity. |
| Governing Laws | Utah Code Title 75 - Utah Uniform Probate Code, specifically sections 75-2-1101 through 75-2-1114, governs Living Wills and Advance Health Care Directives in Utah. |
| Primary Purpose | It serves to communicate an individual’s wishes regarding life-sustaining treatment, including the refusal of or request for specific medical interventions, in the event they are not able to express their preferences due to incapacitation. |
| Requirements for Validity | To be considered valid, a Utah Living Will must be either witnessed by two individuals who are not related to the person by blood, marriage, or adoption and who do not stand to inherit from the person, or it must be notarized. The person creating the living will must also be of sound mind and acting of their own free will. |
How to Write Utah Living Will
Filling out a Utah Living Will form is a prudent step for anyone wanting to ensure their healthcare preferences are respected even when they cannot express themselves due to medical reasons. This document, also known as an advance directive, helps to communicate one's wishes regarding the extent of medical treatment they desire if they become unable to make decisions for themselves. The process of filling out the form is straightforward but requires attention to detail to ensure that all information is accurately conveyed.
- Begin by gathering necessary information, including your full legal name, date of birth, and contact information.
- Read the form thoroughly before you start filling it out. This ensures you understand what each section is requesting and how your responses will dictate your care.
- Enter your personal information at the top of the form, including your name, address, and any other required fields that identify who you are.
- Decide on the specifics of your healthcare wishes, such as the types of life-sustaining treatments you would want or not want, such as artificial hydration, nutrition, or mechanical ventilation.
- Appoint a healthcare proxy, someone you trust to make healthcare decisions on your behalf if you're unable to do so. Provide their full name, relationship to you, and contact information.
- Discuss your wishes with your healthcare proxy to ensure they understand and are willing to respect your healthcare preferences.
- Sign and date the form in the presence of two adult witnesses who are not related to you by blood or marriage and who do not stand to benefit from your estate. The witnesses must also sign and date the form, acknowledging that you have signed it willingly and are of sound mind.
- If required, have the form notarized. Some versions of the Utah Living Will may need to be notarized to be considered legally binding.
- After completing the form, make copies of it. Provide a copy to your healthcare proxy, your primary care physician, and any healthcare facilities where you receive care. Keep the original in a safe but accessible place.
- Remember to review and update your Living Will periodically or if your health situation or healthcare preferences change.
Creating a Living Will is a proactive way to take control of your healthcare decisions and alleviates the burden on family members during challenging times. By clearly stating your medical treatment preferences, you ensure that your wishes are known and can be followed, even when you cannot voice them yourself.