Free Do Not Resuscitate Order Form for Utah
When individuals face serious health concerns, making decisions about emergency medical care becomes crucial. Among these decisions is the choice regarding resuscitation efforts in life-threatening situations, a choice embodied in the Utah Do Not Resuscitate Order form. This document, crucial for those seeking control over their end-of-life care, allows people to state their preference not to receive CPR (Cardiopulmonary Resuscitation) in the event their heart stops or they stop breathing. Acceptance and understanding of this form require navigating its legal and medical implications, as it directly influences the interventions medical professionals will undertake. The form stands as a communication tool between patients, their families, and healthcare providers, ensuring that the patient's wishes are respected at a critical time. By declaring their choice through this form, individuals can have a significant say in their final moments, making its consideration an essential part of healthcare planning in Utah.
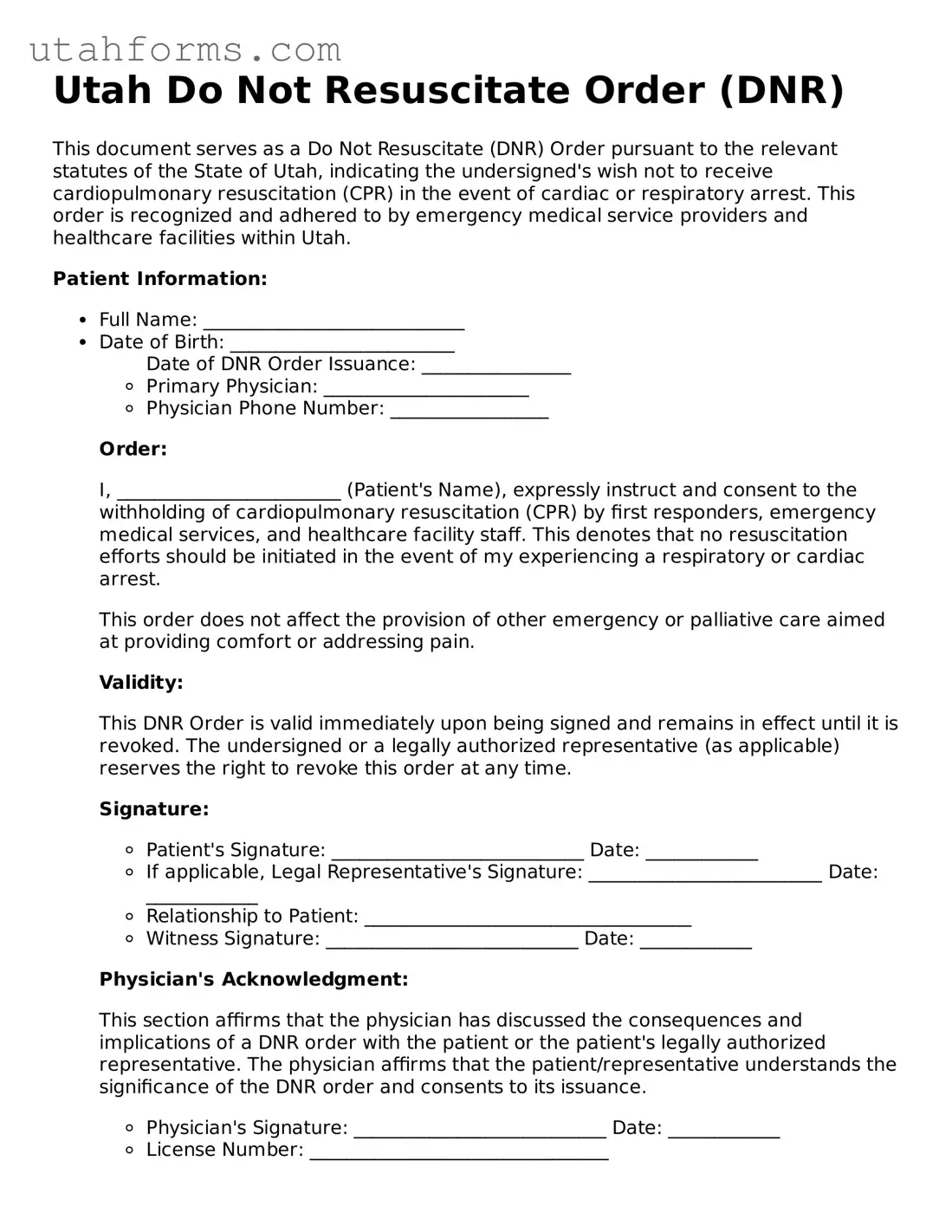
Preview - Utah Do Not Resuscitate Order Form
Utah Do Not Resuscitate Order (DNR)
This document serves as a Do Not Resuscitate (DNR) Order pursuant to the relevant statutes of the State of Utah, indicating the undersigned's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. This order is recognized and adhered to by emergency medical service providers and healthcare facilities within Utah.
Patient Information:
- Full Name: ____________________________
- Date of Birth: ________________________
- Primary Physician: ______________________
- Physician Phone Number: _________________
- Patient's Signature: ___________________________ Date: ____________
- If applicable, Legal Representative's Signature: _________________________ Date: ____________
- Relationship to Patient: ___________________________________
- Witness Signature: ___________________________ Date: ____________
- Physician's Signature: ___________________________ Date: ____________
- License Number: ________________________________
- Date of DNR Order Issuance: ________________
Order:
I, ________________________ (Patient's Name), expressly instruct and consent to the withholding of cardiopulmonary resuscitation (CPR) by first responders, emergency medical services, and healthcare facility staff. This denotes that no resuscitation efforts should be initiated in the event of my experiencing a respiratory or cardiac arrest.
This order does not affect the provision of other emergency or palliative care aimed at providing comfort or addressing pain.
Validity:
This DNR Order is valid immediately upon being signed and remains in effect until it is revoked. The undersigned or a legally authorized representative (as applicable) reserves the right to revoke this order at any time.
Signature:
Physician's Acknowledgment:
This section affirms that the physician has discussed the consequences and implications of a DNR order with the patient or the patient's legally authorized representative. The physician affirms that the patient/representative understands the significance of the DNR order and consents to its issuance.
Document Properties
| Fact | Detail |
|---|---|
| Definition | A Utah Do Not Resuscitate (DNR) Order form is a legal document that communicates a person’s wish not to have CPR (Cardiopulmonary Resuscitation) if their heart stops or they stop breathing. |
| Governing Law | In Utah, DNR orders are governed by the Utah Uniform Patient Act (Utah Code Ann. §§ 75-2a-101 to -111). |
| Who can request? | The form can be requested by the patient themselves, a legal guardian, or a health care proxy, pursuant to the individual’s wishes and applicable state laws. |
| Physician's Role | A licensed physician must sign the DNR Order, validating the patient’s health condition and their decision for the DNR. |
| Eligibility | To be eligible for a DNR Order in Utah, an individual must have a terminal condition or be in a persistent vegetative state, as confirmed by a physician. |
| Effectiveness | The DNR Order becomes effective immediately upon being signed by both the physician and the patient or their authorized representative. |
| Revocation | A DNR Order can be revoked at any time by the patient, their guardian, or healthcare proxy, either verbally or by physically destroying the DNR form. |
| Form Availability | The specific form is provided by healthcare providers, or it can be accessed through the Utah Department of Health or relevant state websites. |
| Emergency Personnel | Emergency medical personnel are required to follow a valid DNR Order when presented with one, provided it complies with all state-specific regulations. |
How to Write Utah Do Not Resuscitate Order
Navigating through the process of filling out a Utah Do Not Resuscitate (DNR) order form is an important step for those who wish to ensure that their wishes regarding emergency medical care are respected. A DNR order is a legal document that tells medical professionals not to perform cardiopulmonary resuscitation (CPR) if a person's breathing stops or if their heart stops beating. Filling out this form precisely is crucial so that healthcare providers can follow an individual’s wishes accurately in critical situations. Here are step-by-step instructions to complete the form correctly.
- Start by obtaining the most current version of the Utah Do Not Resuscitate Order form. Make sure it's the official form used by the state of Utah.
- Read the entire form carefully before you start filling it out. Understand what each section is asking for to ensure that your information is accurately conveyed.
- In the section designated for patient information, enter your full legal name as the patient. Make sure to spell your name correctly and verify that it matches the name on your official ID.
- Fill in your date of birth in the specified format. This typically includes the month, day, and year.
- Provide your address, including street name and number, city, state, and zip code. This helps in identifying your residence for medical personnel if needed.
- Indicate your gender by checking the appropriate box. This information may be used to match medical records and other documents.
- Next, the form requires the signature of the individual issuing the DNR order. If you are the patient, sign in the designated area. If a legal guardian, healthcare power of attorney, or surrogate is signing the form, they must sign and indicate their relationship to the patient.
- Signature of a physician is also mandatory. The physician must review the DNR order, agree that it aligns with the patient’s current medical condition and wishes, and then sign and date the form.
- After the physician's signature, the form might require additional verification such as a witness or notary public signature. Follow the specific instructions if this is required. Notarization helps in further authenticating the document.
- Ensure that all parts of the form are complete and that no required sections are left blank. Missing information could lead to confusion or the form being considered invalid.
- Finally, make copies of the completed Do Not Resuscitate Order form. Keep the original in a safe but accessible place, and consider giving copies to close family members and your healthcare provider(s).
Completing the Utah Do Not Resuscitate Order form is a proactive step towards making your medical wishes known. It's essential to discuss these decisions with loved ones and healthcare providers to ensure they understand your preferences and the reasons behind them. With the form accurately filled out and properly signed, you can feel more secure knowing that your healthcare directives will be respected during critical moments.
Frequently Asked Questions
-
What is a Do Not Resuscitate (DNR) Order in Utah?
A Do Not Resuscitate (DNR) Order in Utah is a legal document that instructs medical professionals not to perform CPR (cardiopulmonary resuscitation) or advanced cardiac life support if a person's breathing or heartbeat stops. This order is typically requested by an individual or their healthcare proxy in anticipation of a life-threatening situation where they prefer not to receive such interventions. The order aims to respect the patient's end-of-life wishes.
-
Who can request a DNR Order in Utah?
In Utah, a DNR Order can be requested by an individual for themselves if they are of sound mind and capable of making their own health care decisions. If the individual is unable to make these decisions, a legally authorized healthcare proxy, such as a durable power of attorney for healthcare, can request a DNR on their behalf. This ensures the individual's healthcare wishes are respected, even if they can't communicate them personally.
-
How is a DNR Order obtained in Utah?
Obtaining a DNR Order in Utah typically involves a discussion with a healthcare provider, who can help assess the individual's eligibility based on their medical condition and end-of-life wishes. The healthcare provider will then complete the necessary paperwork to formalize the DNR Order. It's important for individuals and their families to communicate openly with healthcare providers to ensure that the DNR Order accurately reflects their wishes.
-
Is the Utah DNR Order valid in other states?
The validity of a Utah DNR Order in other states can vary, as each state has its own laws and regulations regarding DNR Orders. If an individual plans to travel or move to another state, it's recommended to check with healthcare providers or legal professionals in that state to determine if the Utah DNR Order will be honored or if a new order needs to be completed.
-
What should be done with the DNR Order once it is completed?
Once a DNR Order is completed in Utah, it should be kept in a place where it can be easily found in an emergency, such as with the individual's other important documents or displayed prominently in their living environment. Copies should also be given to the individual's healthcare proxy, family members, and healthcare providers to ensure the order is followed when necessary.
-
Can a DNR Order in Utah be revoked?
Yes, a DNR Order in Utah can be revoked at any time by the individual or their healthcare proxy if they change their mind about their end-of-life care preferences. Revocation can be done by destroying the DNR document, expressing the wish to revoke the order verbally or in writing, or by performing actions inconsistent with the DNR Order, such as requesting CPR. It's crucial to communicate any change in wishes to all involved parties promptly.
-
Does having a DNR Order affect the quality of other treatments?
Having a DNR Order in Utah does not affect the quality of other treatments an individual may receive. The order specifically addresses the use of CPR and other life-sustaining measures in the event of cardiac or respiratory arrest. Patients with a DNR Order will continue to receive all other appropriate medical care, including pain management and comfort measures, based on their needs and wishes.
Common mistakes
Filling out the Utah Do Not Resuscitate (DNR) Order form is a significant step for individuals and their families. It's crucial to approach this process with care to ensure that your wishes are properly documented and respected. Unfortunately, mistakes can happen. Here are ten common ones that are important to avoid:
- Not checking if the patient is eligible: Eligibility criteria exist for a DNR in Utah. Ensuring the patient meets these criteria before filling out the form is essential.
- Incorrect patient information: A surprisingly common error is the incorrect filling of patient details, such as name, date of birth, or address. Accuracy is vital for proper identification.
- Failing to involve required parties in the decision-making: The decision to enact a DNR involves discussions with family members, healthcare providers, and sometimes legal representatives. Excluding necessary parties can lead to issues down the line.
- Forgetting to have the form signed: A DNR order must be signed by the required individuals, including the patient (if capable) and the healthcare provider. An unsigned form is not valid.
- Lack of witness or notary signatures, when required: Depending on the situation, witness or notary signatures might be necessary. Failing to include these can invalidate the form.
- Not detailing specific medical interventions to be avoided: While the DNR form indicates a desire not to have resuscitative efforts upon cardiac or respiratory arrest, it's also important to specify other interventions the patient might want to decline.
- Using an outdated form: Regulations and forms can evolve. Using the most current version of the DNR form is critical to ensure compliance with current laws and guidelines.
- Incorrect or unclear photocopies: If copies of the form are needed, ensure they are clear and accurate. Unclear or incorrect copies can lead to confusion in emergency situations.
- Not informing family members or caregivers of the DNR order: It’s crucial that family members and other caregivers are aware of the DNR order, understand what it means, and know where the original document is stored.
- Failure to review and update the DNR order: Circumstances and wishes can change. Regularly reviewing and, if necessary, updating the DNR order ensures that the document reflects the current wishes of the patient.
When completing a DNR order, it's beneficial to approach the process with thoroughness and attention to detail. Avoiding these mistakes can ensure that wishes are honored without undue stress on family members and healthcare providers. Resources and guidance from healthcare professionals can be instrumental in navigating this process.
Documents used along the form
When it comes to planning for one's health care, a Do Not Resuscitate (DNR) Order is just one crucial document among many designed to respect an individual's medical and personal wishes. In Utah, as in many places, this legal document prevents emergency medical services (EMS) from performing cardiopulmonary resuscitation (CPR) in the event a person's heart stops or they stop breathing. Alongside a DNR, several other forms often play a pivotal role in ensuring a person's health care directives are clearly communicated and honored. These forms together create a comprehensive approach to end-of-life planning.
- Advance Health Care Directive - This vital document allows individuals to specify their health care preferences should they become unable to make decisions for themselves. It encompasses a wide range of decisions, including the use of life-sustaining treatments and pain management.
- Medical Power of Attorney (POA) - Similar to the Advance Health Care Directive, a Medical POA enables a person to appoint a trusted individual to make health care decisions on their behalf, should they become incapacitated.
- Living Will - While it shares some similarities with the Advance Health Care Directive, a Living Will more specifically documents an individual's wishes regarding end-of-life care and treatments they do or do not want to receive.
- Physician Orders for Life-Sustaining Treatment (POLST) - This form complements a DNR by detailing other types of medical interventions a patient wishes to avoid or receive, beyond just CPR. It is intended for seriously ill individuals for whom death within a year would not be surprising.
- Out-of-Hospital Do Not Resuscitate Order - Specifically designed for use outside of hospital settings, this form ensures that EMS personnel are aware of and comply with an individual's DNR wishes during an emergency.
- Health Care Privacy (HIPAA) Authorization Form - This document allows healthcare providers to share an individual's health information with designated persons, which is critical for healthcare proxies or family members involved in making medical decisions.
- Organ and Tissue Donation Registration - Individuals can specify their intentions regarding organ and tissue donation in this document, ensuring their wishes are known and can be acted upon in the event of their death.
Understanding and completing these forms may seem daunting, but they are crucial in ensuring an individual's healthcare wishes are respected and followed. Each one covers different aspects of one's care and preferences, making them collectively essential for comprehensive health care planning. With these documents in place, individuals, their families, and healthcare providers can all have the clarity and guidance necessary to make informed decisions during challenging times.
Similar forms
The Utah Do Not Resuscitate (DNR) Order is similar to a Living Will, as both documents express the patient's healthcare preferences concerning end-of-life care. A Living Will typically outlines decisions about life-sustaining treatment if a patient becomes terminally ill or permanently unconscious, allowing them to decline certain types of medical interventions. Like a DNR, it is a critical tool for ensuring that a patient's medical treatment aligns with their wishes.
Similar to the DNR is the Medical Power of Attorney (MPOA), which designates an individual to make healthcare decisions on behalf of someone else, should they become unable to do so themselves. This document complements a DNR by providing a broader authority over healthcare decisions beyond resuscitation, including the types of medical treatments and interventions the patient would or would not want to receive.
The POLST (Physician Orders for Life-Sustaining Treatment) form also shares similarities with the Utah DNR. It goes beyond a DNR by providing specific instructions regarding a range of life-sustaining treatments, in addition to CPR. These can include preferences regarding intubation, mechanical ventilation, and artificial nutrition. Like a DNR, a POLST is designed to ensure that healthcare professionals understand and respect the patient's wishes regarding end-of-life care.
Another document similar to the Utah DNR is an Advance Healthcare Directive, which combines elements of a Living Will and Medical Power of Attorney. It allows individuals to outline their healthcare preferences and appoint an agent to make decisions if they are incapacitated. This comprehensive approach ensures that both the patient's treatment preferences and the choice of who makes decisions are clearly documented.
The Five Wishes document also aligns closely with the intent behind a DNR, offering a more detailed and personalized approach to specifying one's healthcare and personal comfort preferences, appointing a healthcare agent, and expressing desires regarding treatment. It is unique in encompassing aspects of personal, emotional, and spiritual needs alongside medical and legal considerations.
A Healthcare Proxy is another document related to the Utah DNR. It specifically allows someone to appoint a healthcare agent or proxy to make medical decisions on their behalf. While it focuses on the appointment of a decision-maker rather than specific medical treatments, its purpose—to ensure decisions respect the patient’s wishes—mirrors the intent of a DNR.
Lastly, the Emergency Medical Services (EMS) Do Not Resuscitate Order shares a direct purpose with the Utah DNR, specifically instructing emergency personnel not to initiate CPR or other resuscitation methods in emergencies. This type of document is crucial for individuals who wish to avoid unwanted resuscitation efforts in situations outside of a hospital or healthcare setting.
Dos and Don'ts
Completing the Utah Do Not Resuscitate (DNR) Order form requires careful attention to detail and an understanding of the implications. Below are essential dos and don'ts to consider during this critical process:
- Do familiarize yourself with the purpose of a DNR. It's a medical order that tells health professionals not to perform cardiopulmonary resuscitation (CPR) if your heart stops or if you stop breathing.
- Do discuss your decision with your family, close friends, and healthcare provider to ensure it reflects your wishes and health care views.
- Do ensure that the form is filled out accurately and completely. Missing information can lead to the form being invalid or not carried out as you wish.
- Don't leave spaces blank. If a section does not apply, it's better to write “N/A” (not applicable) rather than leaving it empty. This shows you didn't overlook the section.
- Don't sign the form without a witness or the necessary healthcare provider's signature, as required by Utah law. The form may not be considered valid without these signatures.
- Do keep the original document in a place where it can be easily found by family or emergency personnel, and consider informing your primary care provider where the original document is kept.
Misconceptions
When discussing the Utah Do Not Resuscitate (DNR) Order form, several misconceptions commonly arise. Understanding these can help clarify its purpose, scope, and implications. Below are six such misconceptions:
Misconception 1: A DNR Order is for the elderly only. The belief that DNR Orders are exclusively for older adults is widespread but incorrect. Individuals of any age with serious health conditions may consider a DNR Order if they wish to avoid certain life-sustaining treatments in the event of cardiac or respiratory arrest.
Misconception 2: Having a DNR means you won’t receive any medical treatment. A common misunderstanding is that a DNR Order eliminates the possibility of receiving medical treatment. In reality, it specifically declines CPR (cardiopulmonary resuscitation) or other resuscitative efforts after heart or breathing stops. It does not affect other treatments that could improve quality of life or provide comfort.
Misconception 3: A DNR Order can be implemented verbally. While communication with healthcare providers about wishes is crucial, in Utah, a valid DNR must be documented on the official Utah DNR Order form. Verbal agreements alone are not sufficient to enforce a DNR decision.
Misconception 4: Only the individual can request their own DNR Order. Although the decision should ideally involve the individual, situations may arise where they cannot make their wishes known due to incapacity. In such cases, family members, healthcare proxies, or legal guardians may be involved in the decision-making process to ensure that the individual’s healthcare preferences are respected, in accordance with state laws.
Misconception 5: A DNR Order is permanent and cannot be changed. This belief is not true. Individuals can review and change their DNR status as their medical condition or preferences evolve. It is important to discuss any changes with a healthcare provider and ensure the DNR Order form is updated accordingly.
Misconception 6: DNR Orders are universally recognized across all states. While many states have reciprocal arrangements recognizing DNR Orders from other states, there can be variations in the legal requirements and forms used. Therefore, it is advisable to review and, if necessary, update the DNR Order according to the regulations of the current state of residence or if planning to move to a different state.
Addressing these misconceptions about the Utah Do Not Resuscitate Order form helps clarify its purpose and ensures that individuals can make informed decisions regarding their end-of-life care wishes. It's crucial for discussions about DNR Orders to be based on accurate information and understanding.
Key takeaways
Filling out and using the Utah Do Not Resuscitate (DNR) Order form carries significant implications for patients and healthcare providers alike. It is a legal document that requires careful attention to both the details and the broader implications of electing not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. Here are four key takeaways to consider:
- Accuracy is paramount: When completing the Utah DNR form, it's crucial that all information is accurate and legible. This ensures that healthcare professionals can readily understand and follow the patient's wishes. Details like the patient's full name, date of birth, and specific medical conditions should be double-checked for correctness.
- Healthcare provider's signature is required: For the DNR order to be considered valid and legally binding in Utah, it must be signed by a licensed healthcare provider. This signature indicates that the healthcare provider has discussed the patient's decision not to undergo CPR with the patient and/or the patient's legally authorized representative.
- Readily accessible documentation: Once completed, the DNR order should be kept in a place where it can be easily accessed by emergency medical personnel. Often, patients are advised to keep a copy on their person (e.g., in a wallet or purse) and in their home in a visible location. This ensures that in the event of an emergency, the document can be quickly found and acted upon.
- Review and update regularly: A patient's medical condition and preferences may change over time. As such, it is recommended that the DNR order be reviewed periodically and updated if the patient's wishes or health status change. Any updates require a new form to be completed and signed by both the patient (or their representative) and the healthcare provider.
Other Popular Utah Templates
Utah Power of Attorney - A proactive step parents can take to manage their child's affairs during travel or extended absence.
Is Utah a 50 50 Divorce State - A legally binding document specifying the conditions under which a couple has agreed to live apart.
Utah Deed Requirements - Indispensable for tax assessment purposes, as it provides authorities with the necessary information to levy property taxes.